Lead Poisoning Detection & Prevention
Lead poisoning is a serious condition, especially in children, affecting brain development and overall health. Even low lead levels can cause harm, making early detection through testing crucial for timely intervention and treatment.
Lead poisoning is a serious condition, especially in children, affecting brain development and overall health. Even low lead levels can cause harm, making early detection through testing crucial for timely intervention and treatment.
Reliable Lead Poisoning Tests for Accurate Diagnosis
Meridian’s reliable lead poisoning tests play a crucial role in early detection and prevention, ensuring timely medical intervention. These tests provide an accurate diagnosis, helping to safeguard children, adults, and at-risk populations from harmful exposure. With quick and precise results, healthcare providers can take necessary steps to reduce long-term health risks. Regular testing with Meridian’s advanced solutions is essential for maintaining overall well-being and preventing complications.
Take Action Before Health and Learning Suffer
Approximately 1 in 3 children worldwide are affected by lead poisoning, making early detection crucial. A blood lead test is the only definitive way to diagnose lead exposure, allowing for timely intervention to reduce long-term health risks. Young children under 6 years old are particularly vulnerable, as lead exposure can impact their development and cognitive growth. Pregnant women should also undergo testing to prevent lead transfer to the unborn child, ensuring a healthier start to life. Additionally, workers in industrial and construction settings are at higher risk and should be regularly tested to mitigate potential health complications.
How Lead Poisoning Affects Health: Key Sources and Risks
Lead Poisoning occurs when individuals come into contact with lead-contaminated sources such as dust, soil, paint, and water. It can impair cognitive development, damage vital organs, and affect overall well-being, especially in children, posing significant public health challenges on a global scale.
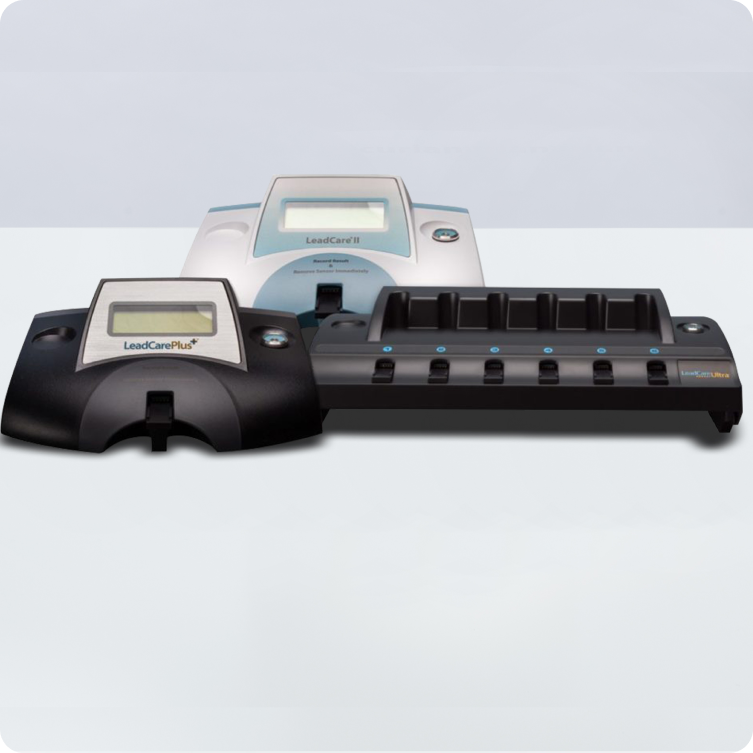
LeadCare Blood Lead Testing is a reliable solution for the early detection of lead poisoning in pediatric and neonatal patients.
It’s more than lead paint. 30% of children are exposed to lead by additional sources.2
There is NO safe level of lead in the blood. Exposure to even small amounts of lead can cause irreversible damage to one’s health.3
In the U.S., about 1 in every 3 housing units may have lead paint hazards.4
Testing Solutions for Lead Poisoning
Point-of-Care Lead Testing Reaches those at Risk, Eliminating the Need for Follow-up.
Meridian Bioscience’s LeadCare platform, a trusted point-of-care testing solution for over 20 years, offers fast and accurate blood lead results in three minutes. Developed in collaboration with the CDC, this portable instrument ensures early detection of lead exposure, facilitating timely intervention to safeguard children's health and prevent long-term developmental and neurological impacts. Early detection through blood lead testing significantly contributes to uncovering those at risk and mitigates ongoing exposure to this harmful neurotoxin.
Learn More About Lead Poisoning
Advancing Lead Poisoning Testing & Prevention for a Healthier Future
At Meridian, we are committed to raising awareness and enhancing early detection through lead poisoning testing and prevention. Lead exposure, especially in children and pregnant women, can cause severe health complications, including developmental delays and neurological issues. Our advanced lead poisoning test solutions provide accurate and timely detection, helping healthcare providers take proactive measures. Beyond diagnostics, we offer educational resources and expert insights to improve testing utilization and public health awareness. By leveraging our expertise, we empower clinicians, laboratories, and communities to combat lead poisoning effectively. Early lead testing is crucial in preventing long-term harm and ensuring a healthier future. Explore our lead poisoning prevention tools and testing solutions to make a meaningful impact. (µg/dl).
Educational Resources for Lead Testing & Prevention
As dedicated partners in enhancing patient care, we take pride in our diverse diagnostic portfolio and go further by offering educational content and tools, leveraging our expertise to boost testing utilization and support our partners comprehensively.
Frequently Asked Questions About Lead Testing
Lead is a naturally occurring heavy metal used in various products and materials. Exposure to lead, even in small amounts, can affect multiple body systems and be particularly harmful to young children.5
Lead exposure occurs when someone inhales lead-containing dust or swallows something that contains lead. Lead-based paint and lead-contaminated dust are the primary sources of exposure for U.S. children. Despite significant progress, lead poisoning remains a top childhood environmental health problem.6
No level of lead in the blood can be defined as safe. An advisory panel of the CDC now recommends that children with blood levels as low as 3.5 μg/dL be identified as having elevated levels and be monitored. Even such low levels may harm a child’s cardiovascular, immunological, and endocrine health, with consequences for that individual and overall public health. While the effects of lead appear to be irreversible, eliminating lead exposure can reduce further damage.7
Toddlers and young children explore with their hands and frequently put them in their mouths. As young children crawl on the floor and reach windows, railings, and walls, they may inhale dust from peeling and chipping lead-based paint or ingest paint chips. Children under six years of age are biologically more sensitive to lead due to rapid brain and organ development, when the body readily takes up lead—mistaking it for calcium. Therefore, children who are low in calcium or have iron-deficient anemia may have an ever-greater lead uptake.8
Adults can become lead poisoned, most frequently from the workplace and hobbies. Lead in adults can affect the central nervous and gastrointestinal systems and can cause chronic kidney disease as well as other health problems.9
Lead exposure is diagnosed through blood lead testing, which measures the amount of lead in the bloodstream. A small blood sample is taken from the finger, heel, or arm. The results indicate the level of lead in the blood, typically measured in micrograms per deciliter (µg/dL). In the United States, federal law requires all Medicaid-enrolled children to be tested at ages 1 and 2 and up to the age of 6 if they have not been tested previously. Beyond this federal requirement, state mandates and guidelines vary. High-risk children, such as those living in older homes or those with a history of pica (eating non-food items), may need more frequent testing.10
If your blood lead level is elevated, several actions may be taken depending on the severity of the exposure and your individual health status. It’s important to follow your healthcare provider’s recommendations closely if you have an elevated blood lead level to protect your health and prevent potential long-term complications associated with lead poisoning.11
- Medical Evaluation: Your healthcare provider will likely conduct further tests and assessments to confirm the elevated blood lead level and evaluate any symptoms or health effects.
- Identifying the Source of Exposure: It’s crucial to identify and eliminate the source of lead exposure. This may involve testing your home, workplace, or other environments where you spend time to pinpoint sources of lead contamination.
- Monitoring: You may require regular blood lead testing to monitor your levels over time and assess the effectiveness of interventions to reduce exposure.
- Treatment if Necessary: In some cases of high blood lead levels or symptoms of lead poisoning, treatments such as chelation therapy may be considered under medical supervision. Chelation therapy involves medications that bind to lead and help remove it from the body.
- Health Management: Your healthcare provider may recommend dietary changes or supplements that can help support overall health and reduce the absorption of lead in your body.
References:
- https://www.unicef.org/reports/toxic-truth-childrens-exposure-to-lead-pollution-2020
- Brown, M.J. (2012). Lead in Drinking Water and Human Blood Lead Levels in the United States. Morbidity and Mortality Weekly Report, August 10 Supplement, 61, 1-9
- https://www.cdc.gov/lead-prevention/about/index.html
- https://www.epa.gov/lead
- https://www.atsdr.cdc.gov/csem/leadtoxicity/what_lead.html
- https://nchh.org/information-and-evidence/learn-about-healthy-housing/health-hazards-prevention-and-solutions/lead/Healthy Homes
- https://www.cdc.gov/lead-prevention/php/news-features/updates-blood-lead-reference-value.html
- https://www.cdc.gov/lead-prevention/risk-factors/index.html
- https://www.nyc.gov/site/doh/health/health-topics/lead-poisoning-adults-and-lead-poisoning.page
- https://www.cdc.gov/lead-prevention/hcp/clinical-guidance/index.html
- https://www.mayoclinic.org/diseases-conditions/lead-poisoning/diagnosis-treatment/drc-20354723